Abstract
In this study, we analyzed the changes occurring in the peripheral blood mononuclear cells (PBMC) during long-term treatment with the Bruton's tyrosine kinase inhibitor ibrutinib in relapsed or refractory (R/R) chronic lymphocytic leukemia (CLL) patients (pts). PBMC populations were assessed by flow-cytometry including CLL cells, Natural Killer (NK) cells, T-cell memory subsets, helper subpopulations (Ths) and regulatory T cell (Tregs) subsets. Peripheral blood samples were collected before start of treatment and at week (wk) 4, 10, 16, 22 and at 8, 12, 24 and 36 months (mo) of treatment.
Eleven pts were included in the study, 8 males and 3 females, with median age 73 years. Nine age- and sex-matched healthy individuals were included as controls. Comparisons between pts and controls were done with the non-parametric Mann-Whitney U test; between follow-up time points and baseline in pts by Wilcoxon rank test for paired comparisons. Simple regression analyses and the Pearson´s rank test were used to estimate the relationship between different cell populations.
Eight pts had high-risk and 3 intermediate-risk disease according to the modified Rai staging system; 8/11 had 17p deletion or TP53 mutation. Three pts had mutated IgHV genes, 3 unmutated, 2 had borderline mutational status (97-98% identity), and 3 were not assessed. Median number of previous treatments was 1 (range 1-4) and median lymphocyte count 45 x 109/L (range 3.1-109.5). At 12 mo, overall response rate was 100%. All pts achieved partial response, with 63% fulfilling all complete response criteria (Hallek M et al, Blood 2018), but for minimal residual disease negativity. Eight pts were still on treatment at 24 mo, 7 pts at 36 mo. Treatment discontinuation was due to: death (n=1), allogeneic transplantation (n=1), disease progression (n=1) and toxicity (n=1). In 3 pts, ibrutinib dose was reduced due to toxicity; the remaining pts stayed on full-dose (420 mg/day p.o.) during the whole treatment period. At study entry, eight pts had hypogammaglobulinemia but none had ongoing IgG replacement therapy. Of these, 5 started IgG replacement therapy during treatment. All 11 patients experienced G2 infections.
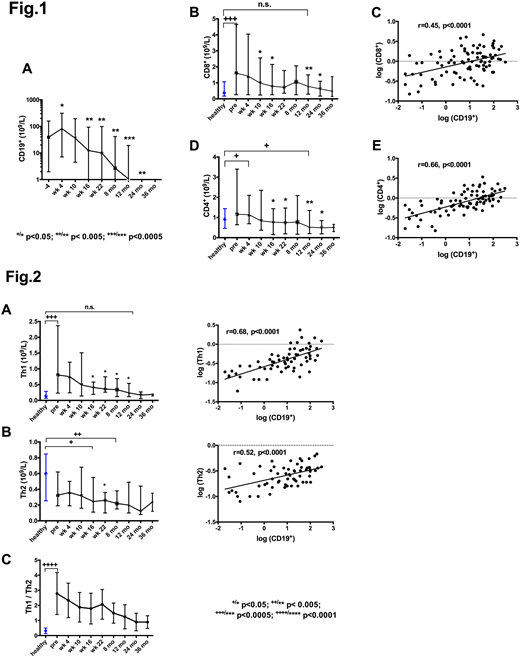
After an initial increase in circulating CLL cells due to redistribution lymphocytosis, a gradual reduction occurred during treatment becoming significant at wk 16 (p<0.005) (Fig. 1A). As we previously reported (Palma M et al, ASH abs 4322, 2017), at study entry CD8+cells were significantly higher compared to controls (p=0.0005). CD8+cells started to decrease at wk 10 (p=0.02) and normalized (i.e. reached values not significantly different from controls) by 12 mo (Fig. 1B). On the other hand, CD4+T cells, at baseline not significantly different from controls, decreased also gradually from wk 16, reaching by 24 mo levels below normal (p=0.02) (Fig.1D).
We show here that the reduction of CD8+ cells correlated with that of CLL cells (r=0.45, p< 0.0001) (Fig. 1C) and that the correlation between the number of CD4+ cells and CLL cells was even more significant (r=0.66, p< 0.0001) (Fig.1E). The expression of the immune checkpoints PD-1 and CTLA-4, at baseline aberrantly high on both CD4+ and CD8+ cells and mainly in the antigen-experienced subsets, decreased gradually during treatment.
Among the helper subsets, Th1 (CCR6-/ CXCR3+) cells were at baseline higher compared to controls (p=0.0003), while Th2 (CCR6-/ CXCR3-) did not significantly differ (Fig.2A-B). As expected, this resulted in a Th1/Th2 ratio significantly higher than in controls (median 2.6 vs 0.26, p<0.0001) (Fig.2C). During treatment, both Th1 and Th2 cells decreased. Th1 normalized by 12 mo, while Th2 cells decreased below normal levels at 12 mo (p=0.006). However, Th1/Th2 ratio never normalized during 36 mo of treatment. The strongest direct correlation was between the decrease of Th1 cells and CLL cells (r=0.68, p< 0.0001). During treatment, NK cells decreased and also Tregs (CD4+/CD25+/ CCR4+/CD127low), in particular the Ag-experienced non-activated subset (CD45RO+HLA-DR-).
In conclusion, the reduction of tumor burden directly correlated with the reduction of all T-cell subsets, but most significantly with those subsets involved in the antitumor immune response, i.e. CD8+cells and, among the CD4+subset, Th1 cells. Whether these changes also compromised the anti-infection immunity is difficult to assess, due to the fact that most of the pts had also underlying hypogammaglobinemia.
Palma:Takeda Pharma AB: Research Funding. Österborg:Gilead: Consultancy, Research Funding; Beigene: Research Funding; Pharmacyclics: Research Funding; Janssen: Research Funding; Abbvie: Research Funding. Mellstedt:Kancera AB: Consultancy, Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Research Funding; Sandoz: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria; Astra-Zeneca: Equity Ownership; Novo Nordisk: Equity Ownership; Global Health Sciences: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal